The Myth of Bad Cholesterol

Disclaimer: I'm not a medical doctor, this is not health advice, do your own research, consult with a qualified physician before making health decisions, caveat emptor, your mileage may vary, yada yada yada.
Let me begin by saying that I find it ridiculous to be writing this post. I'm only here because I suspected my primary care physician was acting in their own best interests rather than my best interests. That suspicion took me down a fascinating rabbit hole.
I had my annual physical recently, which included a standard lipid panel. I got a call from my physician the next day.
"Your cholesterol is extremely high. We need to start you on statins immediately."
Oof. I was expecting a high cholesterol result, as it's been elevated the past couple years as a result of my ketogenic diet. But this score was even higher and I haven't been on keto for several months due to my personal trainer putting me on a diet designed for gaining muscle mass. What were my scores?
- LDL-C: 209 mg/dL
- HDL-C: 90 mg/dL
- Total: 299 mg/dL
Where does that (allegedly) put me in terms of risk?
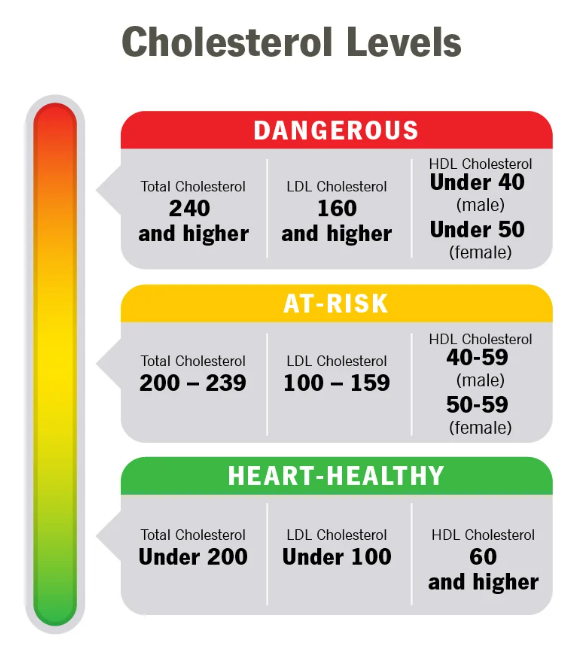
In other words:
- LDL: DANGEROUS
- HDL: healthy
- Total: DANGEROUS
What is "Good" and "Bad" Cholesterol?
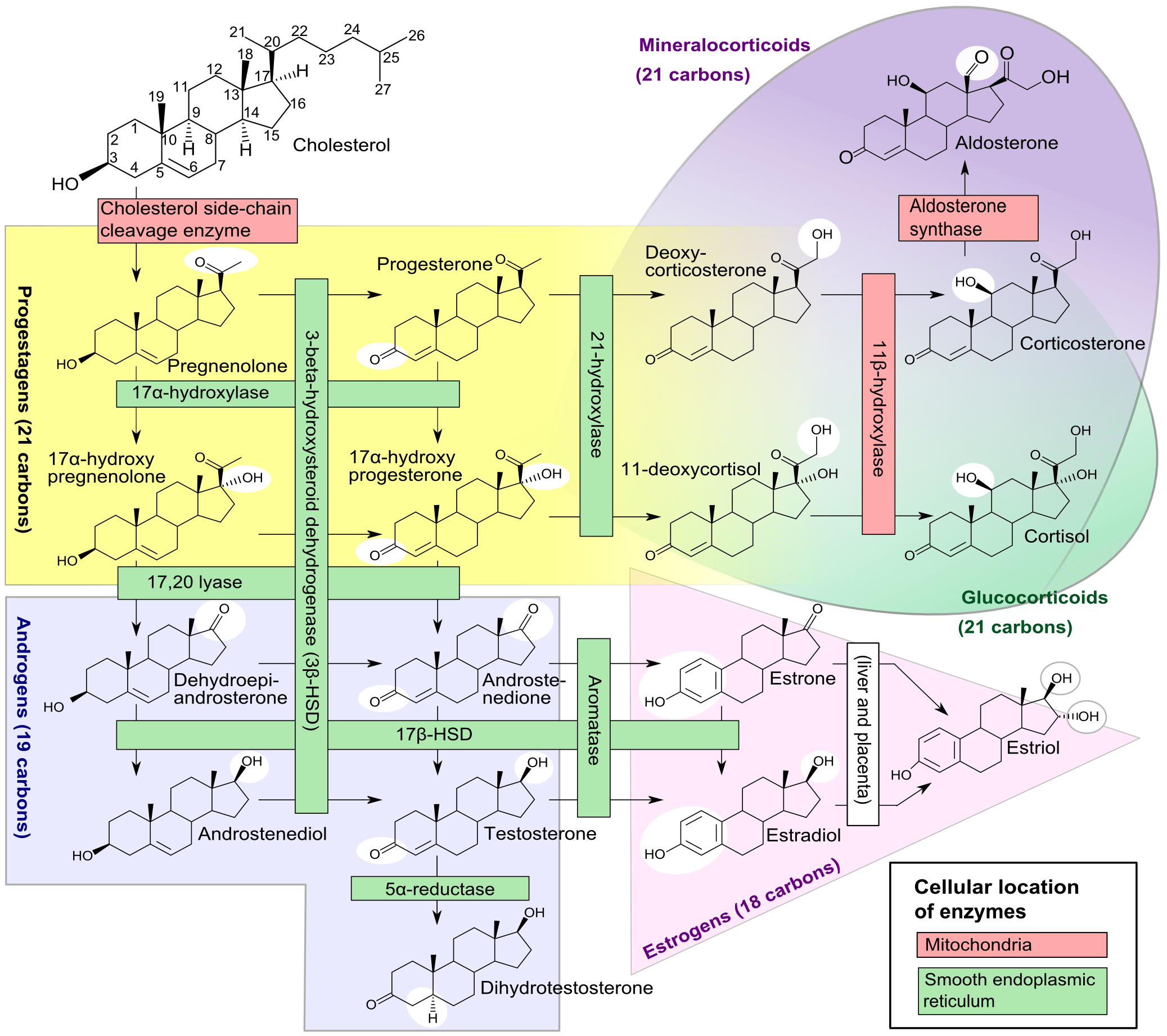
According to the CDC: cholesterol travels through the blood on proteins called lipoproteins. Two types of lipoproteins carry cholesterol throughout the body:
- LDL (low-density lipoprotein) cholesterol, sometimes called “bad” cholesterol, makes up most of your body’s cholesterol. High levels of LDL cholesterol raise your risk for heart disease and stroke.
- HDL (high-density lipoprotein) cholesterol, sometimes called “good” cholesterol, absorbs cholesterol in the blood and carries it back to the liver. The liver then flushes it from the body. High levels of HDL cholesterol can lower your risk for heart disease and stroke.
When your body has too much LDL cholesterol it can build up on the walls of your blood vessels. This buildup is called “plaque,” and it can cause health problems, such as heart disease and stroke.
The above is the explanation that you'll receive from almost every primary care doctor you talk to when reviewing a standard lipid panel. It's also wrong, due to oversimplification and/or ignorance of improvements in our understanding of cholesterol over the past ~20 years.
A Nuanced Modern Take on Cholesterol
Plasma cholesterol levels (which is what clinicians measure with standard cholesterol tests) often have little to do with cellular cholesterol, especially artery cholesterol, which is what we really care about.
Cholesterol is absolutely vital for our existence - it is one of the main building blocks used to make cell membranes. 80% of the cholesterol in your body is PRODUCED by your body - only about 20% comes from food you ingest.
Describing LDL as "bad" and HDL as "good" is a gross oversimplification. "Bad" cholesterol is ANY cholesterol that ends up inside of the wall of an artery AND leads to an inflammatory cascade which results in the obstruction of that artery. When one measures cholesterol in the blood we do not know the final destination of those cholesterol molecules!
According to the Mayo Clinic, Low-density lipoprotein particle (LDL-P) concentration is positively associated with increased risk of atherosclerotic cardiovascular disease (ASCVD). LDL-P is heterogeneous and contains many lipids and proteins, including phospholipids, triglycerides, and cholesterol. LDL cholesterol is a surrogate biomarker of LDL-P.
LDL cholesterol is the historical measure of atherogenic lipid burden. There is a large variance in the relative amount of cholesterol carried by each LDL particle. Consequently, subjects with similar LDL cholesterol values can have markedly different serum concentrations of LDL particles. Multiple studies have shown that serum concentrations of LDL-P more accurately reflect actual risk of ASCVD when LDL cholesterol values are discrepant.
High-density lipoprotein particle (HDL-P) concentration is inversely associated with risk of ASCVD. HDL cholesterol is also inversely associated with ASCVD, since it is a surrogate marker for HDL-P. Like other lipoproteins, HDL-P is heterogeneous, and particles contain highly variable proportions of proteins and lipids, including phospholipids, sphingolipids, and cholesterol.
Several large clinical studies have shown that HDL-P is more significantly associated with ASCVD risk than HDL cholesterol. Furthermore, HDL-P remains significantly associated with ASCVD even among subjects taking cholesterol-lowering medications. HDL-P more accurately reflects actual risk of ASCVD when HDL cholesterol values are discrepant.
Most clinicians focus on LDL-C because it's a good way to predict heart attack risk. But many people diagnosed with heart disease have LDL levels that aren't especially high. It turns out that LDL particles are not all created equal. Smaller, more tightly packed LDL has an easier time getting into arteries. Larger, fluffier particles appear to be less dangerous.
Additionally, research suggests that a key protein on LDL called apolipoprotein B (ApoB) is an important contributor for heart disease risk. When we measure ApoB, we’re actually counting all of these particles that cause plaque buildup, and this is a much more accurate way of determining cardiovascular risk.
Dr. Peter Attia wrote a 9 part series on cholesterol back in 2012. I credit him with giving me the knowledge (from reading his book Outlive) to push back against my primary care physician's knee-jerk response to my high LDL-C test result.
Dr. Attia makes quite a claim (that I find believable after my own personal experience):
By the end of this series, should you choose to internalize this content (and pick up a few homework assignments along the way), you will understand the field of lipidology and advanced lipid testing better than 95% of physicians in the United States. I am not being hyperbolic.
If you're willing to devote an hour or so, I highly recommend reading the whole series. But I cover my high level takeaways in this article.
My Advanced Test Results
After my initial lipid panel, I asked my physician for further testing because I was unconvinced by a single high LDL-C score. The first thing we did was schedule a CT scan of my heart to quantify how much cholesterol had gotten stuck in my arteries.
What was my coronary artery calcification score? 0. Zero. Zed. Zilch. Zip. No measurable amount of cholesterol has gotten stuck in my arteries. This was a good start, but it only showed us a backward-looking metric of damage rather than a forward-looking predictor of damage risk.
So I asked for a referral to a specialist in lipidology. Of course, I was told it would take months to get an appointment. Thankfully, there are plenty of options to get your own bloodwork done quickly (out of pocket) if you wish to route around the healthcare bureaucracy of the United States. Note that if you have an HSA or FSA you may be able to use those tax advantaged funds to pay for the lab work. A few options:
- https://directlabs.com/
- https://www.healthlabs.com/
- https://www.questhealth.com/
- https://www.ultalabtests.com/
After a month of going back and forth with my doctor, I ordered a comprehensive lipid panel, got my blood drawn the next day, and received all my results back within a few days. This was an excellent experience and I'll likely make this a part of my personal annual health assessment.
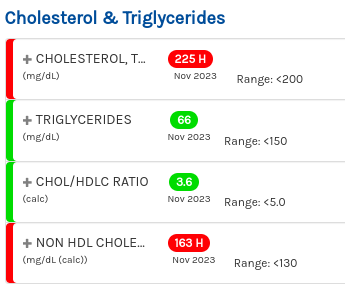
Here we can see the simple metrics that my "total cholesterol" is considered too high, though my triglycerides and actual ratio of LDL to HDL is quite good.
Here we can see that all of my HDL metrics are great.
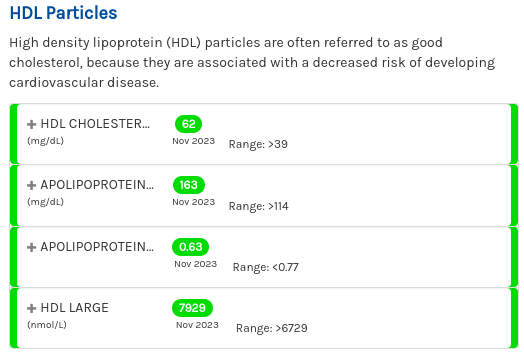
Does having lots of HDL particles help? According to Dr. Attia: probably, especially if they are “functional” at carrying out reverse cholesterol transport, but it’s not clear if it matters when LDL particle count is low.
According to the Mayo Clinic, my LDL-C from a month prior (209 mg/dL) indicated "a likely genetic condition" but now my score of 147 mg/dL is just "borderline high." Coolcoolcool. Why did my LDL-C drop by so much in just 1 month? Well, upon getting the initial 209 score back I immediately re-assessed my new diet in terms of cholesterol and realized that I was consuming a ton of dairy (milk and cheese) and also some of my protein choices had not been great in terms of cholesterol content (chicken thighs over chicken breasts, for example.) So I cut dairy almost completely and am sticking to lower cholesterol cuts of meat.
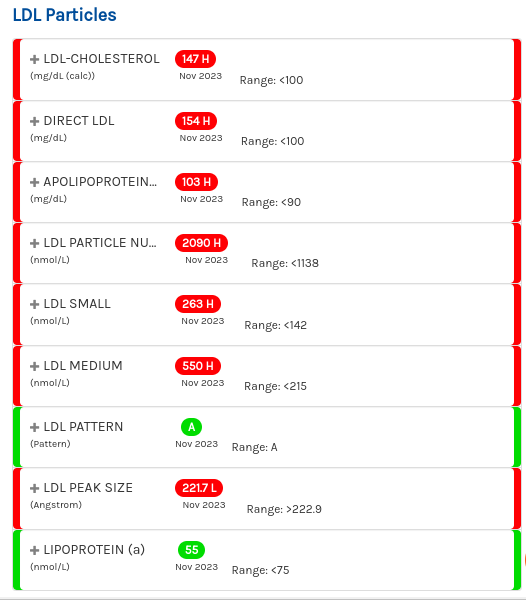
Here's where things get interesting, and it's really a mixed bag. On one hand, my particle counts and number of small particles are higher than I'd like.
The risk ranges for ApoB don't seem to have consensus. Normal range according to Cleveland Clinic for males is 66 to 133 mg/dL. Mine came in a 103 mg/dL which my lab testing provider scored as "moderate risk" for cardiovascular disease. Some cardiology guidelines recommend a target of less than 65 or 80 mg/dL of Apo B. So it's not bad, but I'd like to see it lower.
What makes this all the more confusing is my LDL pattern. If your LDL pattern is classified as Pattern A, it means that the LDL particles in your blood are predominantly large and buoyant. This pattern is generally considered to be less atherogenic, meaning it is less likely to contribute to plaque build-up in the arteries compared to Pattern B, which consists of smaller, denser LDL particles. Pattern A is often associated with a lower risk of cardiovascular disease.
How is this even possible for my number of small particles to be too high and yet overall my particle size pattern is considered large? My theory is that because my LDL-C is so high, it's possible for me to have more small particles than is desirable while also having more large particles than small particles. I suppose I'll have to wait several months for a specialist to explain this phenomenon. So, in summary:
- My LDL-C is high (bad)
- My HDL-C is great
- My ApoB is good but could be better (lower)
- My small LDL particles are high (bad)
- In general my LDL particle size is good (large)
ApoB vs Particle Size
According to this Quebec Cardiovascular Study published in 1997, ApoB came out as the best and only significant predictor of heart disease risk while LDL particle diameter as did not contribute to the risk after the contribution of ApoB levels had been considered. In other words, you only need to worry about if your particle size if you know that your ApoB levels are high. If ApoB is high but your particle sizes are large, your risk is still relatively low.
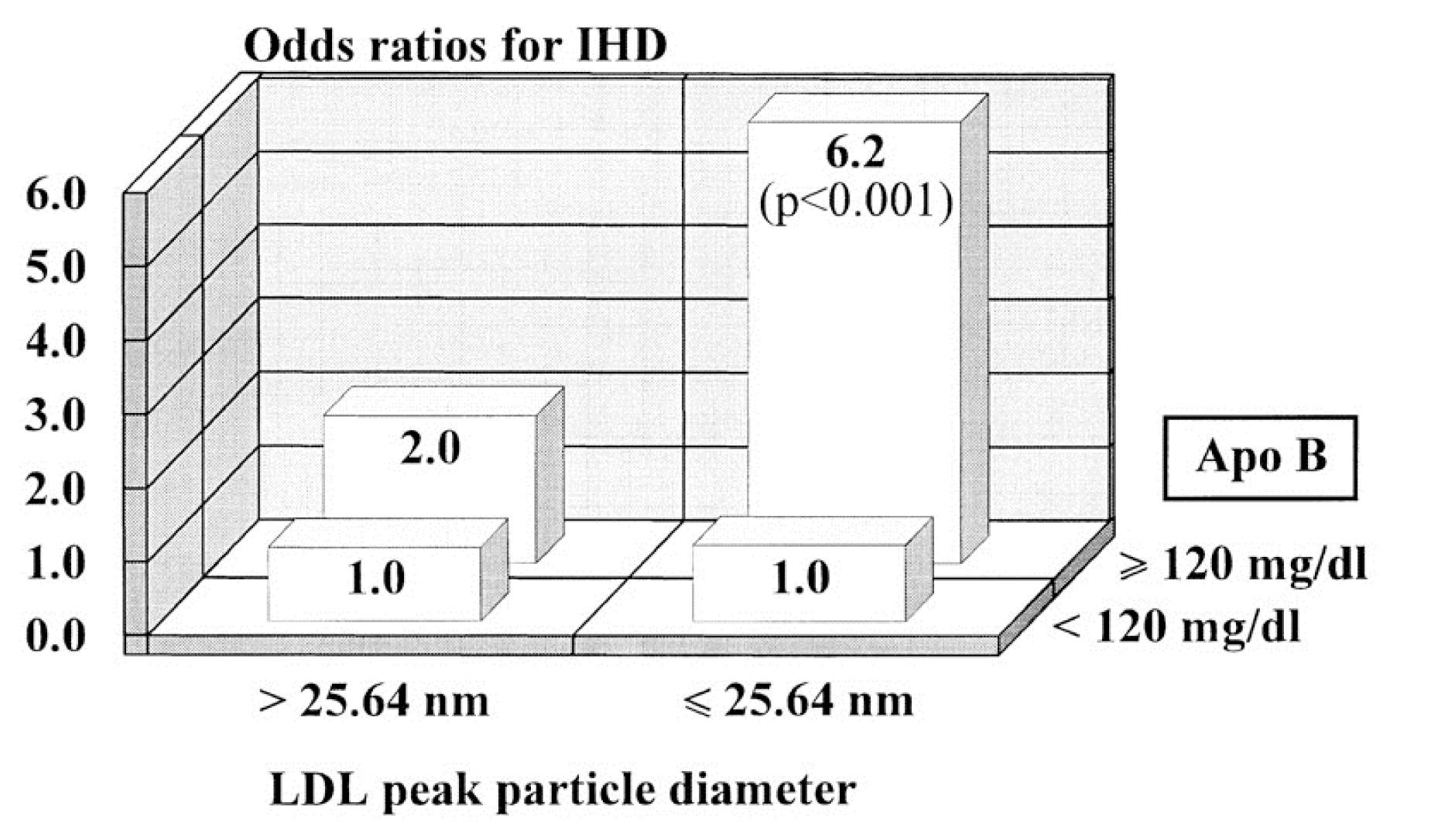
So why does having an LDL-P of 2,000 nmol/L (95th percentile) increase the risk of atherosclerosis relative to, say, 1,000 nmol/L (20th percentile)? In the end, it’s a probabilistic game. The more particles – NOT cholesterol molecules within the particles and not the size of the LDL particles – you have, the more likely the chance a LDL-P is going to squeeze into the sub-endothelial space in your artery wall and begin the process of atherosclerosis. So the primary takeaways here:
- Small LDL particles are more atherogenic than large ones, independent of number.
- The number of particles is what increases atherogenic risk, independent of size.
- Both size and number matter, and so the person on the right is “doubly” at risk.
Can one increase LDL Particle size?
Although LDL cholesterol particle size is mainly genetically inherited, individuals who have small LDL particles can increase their particle size through diet, exercise, and medications.
Diets that are low in saturated fat and cholesterol, regular aerobic exercise, and loss of excess body fat have been determined to decrease the number of small LDL particles and increase the number of large LDL particles in the blood.
When lifestyle changes alone are unsuccessful, medications can be used. Even though statin medications are effective in lowering the absolute levels of LDL cholesterol, they appear to have a limited effect on LDL cholesterol particle size. Medications such as nicotinic acid (niacin) and gemfibrozil (Lopid) have been found effective in many instances in increasing the size of LDL cholesterol particles.
Interestingly, this meta-analysis of 38 randomized trials concluded that the available evidence indicates that dietary interventions restricted in carbohydrates increase LDL peak particle size and decrease the numbers of total and small LDL particles. In other words, ketogenic diets appear to reduce this particular risk factor of arteriosclerosis.
According to this meta-analysis of 36 LDL-P studies, statins, estrogen replacement therapy, and a low fat/high carbohydrate diet lower the LDL-C content in LDL particles more than they lower the LDL-P concentration, while fibrates, nicotinic acid (niacin), exercise, and a low carbohydrate diet lower LDL-P concentration more than they lower LDL-C content. Thus you'd probably want to focus on the latter to achieve the best results.
C-reactive Protein
Several months later I had a different set of tests run and one of them included a measure of my C-reactive protein. According to the Mayo Clinic:
C-reactive protein (CRP) is a protein made by the liver. The level of CRP increases when there's inflammation in the body. High inflammation increases the risk of coronary artery disease, which is when arteries of the heart narrow. Narrowed arteries can lead to a heart attack.
My C-reactive protein result came in at 0.8 mg/L; anything below 1.0 mg/L is considered at low risk of cardiovascular events.
Non-pharmaceutical Remediations for Keto Diets
The BJJ Caveman published a series of posts about his own cholesterol issues while on keto back in 2015. They developed this game plan that seemed to work pretty well according to his follow-up with the results. What was the plan?
- Reduce saturated fats
- Eat more beans (as a probiotic)
- Reduce coffee intake because Cafestol, a compound found in coffee, can stimulate increased cholesterol synthesis by the liver by suppressing bile acid production.
- Increase fiber intake
- Probiotics
- Berberine
- Citrus Bergamot
- Omega 3
Thomas Dayspring has a great (and highly technical) article on high LDL cholesterol and low carb diets: "Lipidaholics Anonymous Case 291 Can losing weight worsen lipids?".
The driving force of atherogenesis is entry of ApoB particles and that force is driven primarily by particle number, not arterial wall inflammation.
Peter Attia's take on people sensitive to saturated fat:
However, some readers may interpret the data I present to mean it’s perfectly safe to consume, say, 25% (or more) of total calories from SFA. I realize I may have to turn in my keto-club card, but I am convinced that a subset of the population—I don’t know how large or small, because my “N” is too small—are not better served by mainlining SFA, even in the complete absence of carbohydrates (i.e., nutritional ketosis). Let me repeat this point: I have seen enough patients whose biomarkers go to hell in a hand basket when they ingest very high amounts of SFA. This leads me to believe some people are not genetically equipped to thrive in prolonged nutritional ketosis.
Peter Attia, "Random finding (plus pi)".
Takeaways
- LDL-P is the best predictor of adverse cardiac events. A high particle count means the particle size is smaller, which means they are more likely to get stuck in your arteries.
- LDL-C is only a good predictor of adverse cardiac events when it is concordant with LDL-P; otherwise it is a poor predictor of risk.
Test frequently! Annual tests are a bare minimum; if you're concerned about your cholesterol then you'll probably want more data points so that you can follow the trend. Remember that it takes decades to develop heart disease so if you catch signs early, you don't need drastic action.
My personal cholesterol situation is clearly complex - it's not the statin-inducing emergency that my primary care doctor made it out to be, but there is clearly room for improvement.
We can see from this 15 year study of 2,500 people that while low LDL-P + high LDL-C comes with pretty good long-term chances of survival, it is slightly better to have low LDL-C as well.
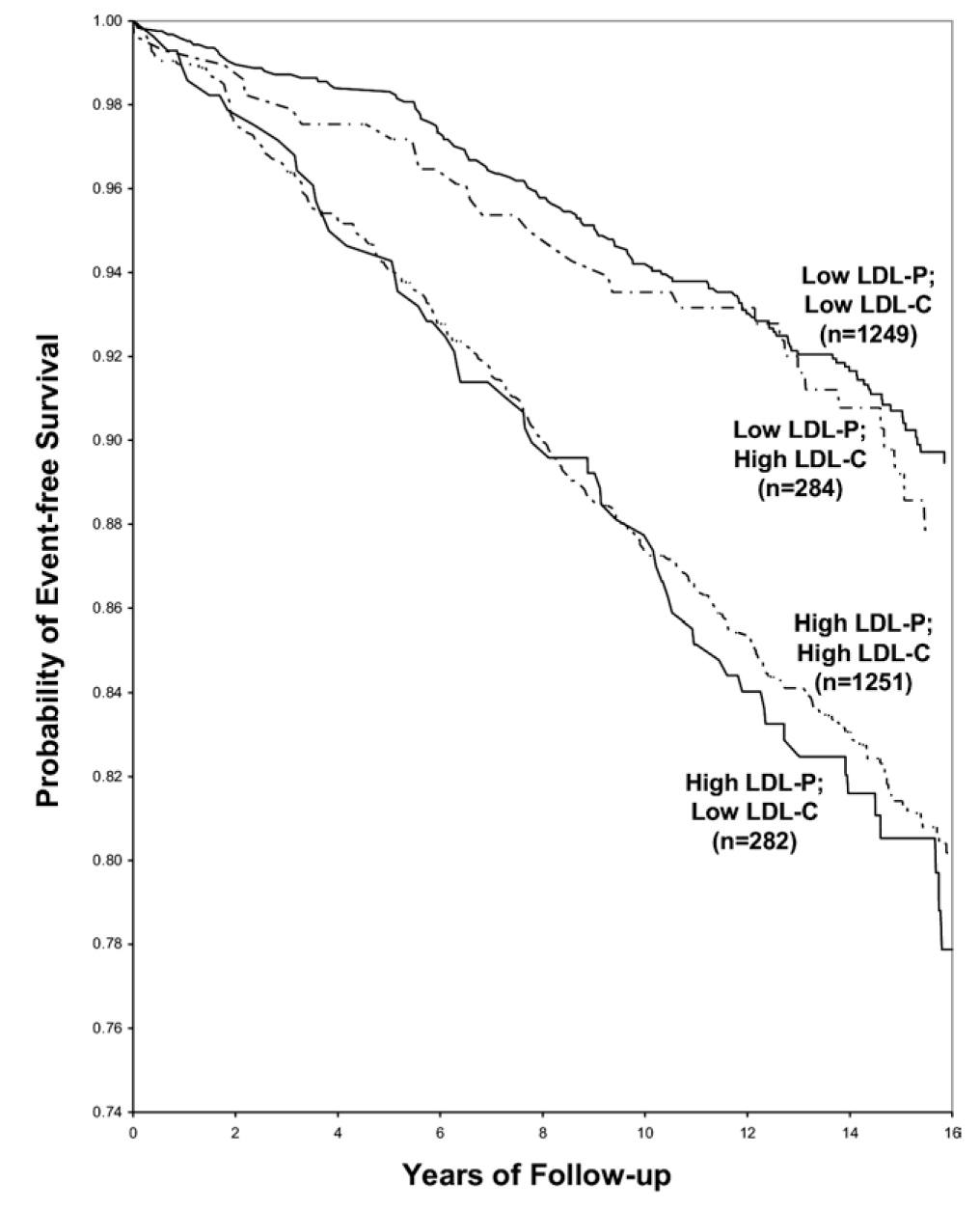
I already dropped my LDL-C score by 60 in one month by cutting my dairy intake. Next I'll take more care to consume less saturated fat, fewer carbohydrates (my trainer suggests carb cycling and only doing 2 high carb days per week), and eat more fibrous vegetables.
Fingers crossed; you only live once!